Lambert-Eaton Myasthenic Syndrome
Synonyms of Lambert-Eaton Myasthenic Syndrome
-
Eaton-Lambert syndrome
-
Lambert-Eaton syndrome
-
LEMS
-
myasthenic syndrome of Lambert-Eaton
General Discussion
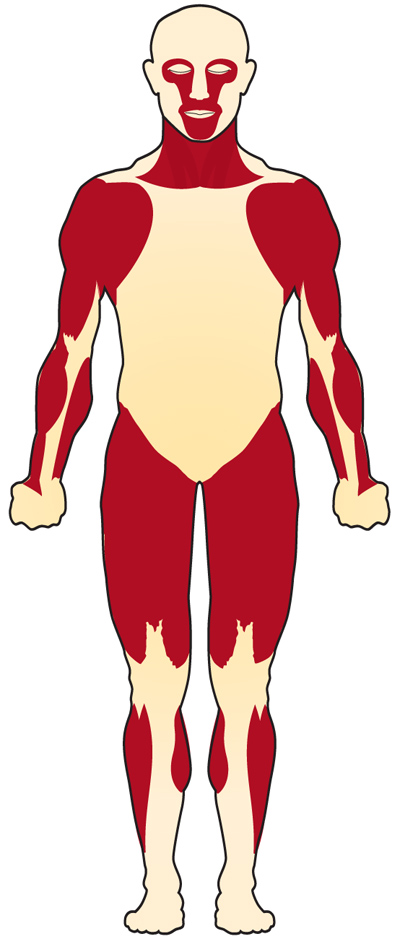
Lambert-Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder of the neuromuscular junction. It is a miscommunication between the nerve cell and the muscles that lead to the gradual onset of muscle weakness. It starts in the proximal muscles of the legs or arms. LEMS can be categorized into two different classes: LEMS associated with small cell lung cancer (SCLC) and LEMS without cancer association. Approximately 60 percent of patients with LEMS have SCLC, and the onset of LEMS symptoms often precedes the detection of the cancer. LEMS patients with cancer tend to be older -predominantly males- and nearly always have a long history of smoking. In patients in which there is no associated cancer, disease onset can be at any age and are gender neutral. LEMS may impact quality of life depending on the severity of symptoms an individual presents with.
Signs & Symptoms
LEMS is characterized by weakness and fatigue especially of the muscles in the legs and arms. The disease may affect the patient’s ability to engage in strenuous exercise and may make such activities as climbing stairs or walking up a steep walkway difficult. Onset is gradual, typically taking place over several weeks to many months. There is often a progression of symptoms whereby the shoulder muscles, muscles of the feet & hands, speech & swallowing muscles and eye muscles are affected in a stepwise fashion. The symptoms progress more quickly when LEMS is associated with cancer. Most LEMS patients also exhibit the following symptoms (sometimes called autonomic symptoms): dry mouth, dry eyes, constipation, impotence, and decreased sweating. LEMS patients with or without cancer may also undergo significant weight loss. The tendon reflexes are diminished or absent on examination. Hence, in summary, LEMS is often described as a clinical “triad” of proximal muscle weakness, autonomic symptoms and reduced tendon reflexes.
Causes
LEMS is an autoimmune disorder. Autoimmune disorders are caused when the body’s natural defenses against “foreign” or invading organisms (e.g., antibodies) begin to attack healthy tissue for unknown reasons. LEMS occurs because autoantibodies damage the “voltage-gated calcium channels (VGCC)” on the motor nerve membrane at the neuromuscular junction. These channels normally conduct calcium into the nerve resulting in release of a chemical known as acetylcholine. Acetylcholine helps in the communication between nerve cells and muscles and is one of a group of chemicals known as neurotransmitters, which help to transmit nerve impulses. The autoantibodies attack the VGCC resulting in less acetylcholine release.In patients who have LEMS associated with cancer, the immune mediated response is initiated because VGCC are present on the surface of cancer cells and the immune system triggers the production of antibodies to fight off cancer cells. The idea is that autoantibodies created against the VGCC on the small cell lung cancer mistakenly attack the VGCC on the nerve membrane instead. One of the major risk factors for SCLC is smoking, and in patients who have LEMS associated with cancer, a long history of smoking is also a major contributing factor.In people who have LEMS not associated with cancer, genetic associations have been made with human leukocyte antigen (HLA) genotypes. HLA are proteins also present on the cell surface, and their function is to regulate the human immune system. However, it is unknown what causes these proteins to go awry array and trigger autoantibody production.
Affected Populations
The estimated worldwide prevalence of LEMS is about 2.8 per million, making it a rare disease. There are approximately 400 known cases of LEMS in the United States. When LEMS is associated with SCLC, the patients tend to be older and are more likely to be men than women. The average age of onset of SCLC is around 60 years of age. Approximately 3% of SCLC patients develop LEMS, but clinical symptoms of LEMS usually precede the SCLC diagnosis (sometimes by many years). When LEMS is not related to cancer, the syndrome may occur at any age, and the typical onset is about 35 years of age. LEMS is extremely rare in the pediatric population, and there have only been 11 affected children reported in literature.
Related Disorders
Diagnosis
Diagnosis of LEMS is based on clinical symptoms and signs. A few diagnostic testing methods are available to help diagnose LEMS. Electrophysiological studies, are done to measure muscle response and muscle strength. Repetitive nerve stimulation measures the electrical activity of the muscle upon stimulation. Antibody testing is done in order to identify the presence of anti-VGCC antibodies.Electromyography results usually show a decrease in compound motor action potential (CMAP). Repetitive nerve stimulation initially shows a small amount of electrical activity in the muscle. After high frequency repetitive stimulation or exercise, there is increased activity in the muscle.Anti-VGCC antibodies are detectable in approximately 85% of LEMS patients and when detected they are highly specific for the condition. This is because anti- VGCC antibodies are found in LEMS with SCLC and in LEMS without cancer association.Screening for SCLC is a very important part of the diagnostic workup for LEMS. A chest CT (and sometimes FDG-PET) scan will usually form the basis of this screening. Depending on the risk profile, a negative initial screen will be repeated at suitable time intervals. A recently discovered tumor marker antibody directed against SOX, which is found in 65% of SCLC LEMS patients as opposed to only 5% of non-tumor LEMS patients, may help guide clinical practice in the future.
Treatment
Treatment of LEMS may vary depending upon the presence of associated cancer. If cancer is present, treatment first involves treatment directed at the cancer, this alone may result in relief of LEMS symptoms.There is no cure for LEMS and treatment usually involves improving quality of life. Therefore, symptomatic treatment is the focus in the management of LEMS. The FDA recently approved a new drug for the symptomatic relief of symptoms associated with muscle weakness called Firdapse (amifampridine). It is a potassium channel blocker that works by increasing the release of acytelcholine. At this time, it is the only drug approved for the indication of LEMS. The medication has shown to have significant benefits such as improving muscle strength and CMAP. In addition, it is a well-tolerated medication.If Firdapse alone does not improve symptoms, there are additional options that can be added in case of symptom progression. Mestinon is indicated for the treatment of MG, but is often used in combination with Firdapse to treat symptoms of autonomic dysfunction (dry mouth, dry eyes, constipation, impotence and, decreased sweating). In MG, Menstinon improves muscle strength, but in LEMS, it has only shown to improve symptoms of autonomic dysfunction.In 2019, Ruzurgi (amifampridine) was approved to treat LEMS in patients 6 to less than 17 years of age. This is the first FDA approved treatment specifically for pediatric patients with LEMS.Drugs that suppress the activity of the immune system (immunosuppressive drugs) are used in LEMS patients with more severe symptoms, e.g. prednisone (alone or in conjunction with azathioprine or cyclosporin). In some patients, a course of high dose immunoglobulins may prevent further disease progression.
Resources:
https://rarediseases.org/rare-diseases/lambert-eaton-myasthenic-syndrome/
https://www.mda.org/disease/lambert-eaton-myasthenic-syndrome
https://myastheniagravisnews.com/sponsored-articles/2021/09/13/is-your-mg-actually-lems/
Myasthenia Gravis
MG is a chronic autoimmune neuromuscular disorder characterized by weakness of the voluntary muscle groups, which are the muscles we use to perform physical activities. For reasons that are not clearly understood, the immune system of patients with MG makes antibodies against the receptor sites of the neuromuscular junction.
Multifocal Motor Neuropathy
MMN (Multifocal Motor Neuropathy) is a rare disorder in which focal areas of multiple motor nerves are attacked by one’s own immune system. Typically, MMN is slowly progressive, resulting in asymmetrical weakness of a patient’s limbs.
CIDP
Chronic Inflammatory Demyelinating Polyneuropathy (CIDP) is a neurological disorder characterized by gradually (over months or years) increasing weakness of the legs and arms. It is caused by damage to the protective covering of the nerves, called myelin. Symptoms are variable and may be mild to debilitating.
Guillain-Barré Syndrome
Guillain-Barré syndrome (GBS) is a rare neurological disorder in which the body’s immune system mistakenly attacks part of its peripheral nervous system—the network of nerves located outside of the brain and spinal cord.
Myositis
Myositis means inflammation of the muscles that you use to move your body. An injury, infection, or autoimmune disease can cause it. Two specific kinds are polymyositis and dermatomyositis. Polymyositis causes muscle weakness, usually in the muscles closest to the trunk of your body. Dermatomyositis causes muscle weakness, plus a skin rash.
Lambert-Eaton Myasthenic Syndrome
Lambert-Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder of the neuromuscular junction. It is a miscommunication between the nerve cell and the muscles that lead to the gradual onset of muscle weakness.
Amyotrophic Lateral Sclerosis
Amyotrophic lateral sclerosis (ALS) is a group of rare neurological diseases that mainly involve the nerve cells (neurons) responsible for controlling voluntary muscle movement (e.g. chewing, walking, and talking). The disease is progressive, and symptoms get worse over time. Currently, there is no cure for ALS and no effective treatment to halt, or reverse, the progression of the disease.
Muscular Dystrophy
Muscular dystrophies are a group of muscle diseases caused by mutations in a person’s genes. Over time, muscle weakness decreases mobility, making everyday tasks difficult. There are many kinds of muscular dystrophy, each affecting specific muscle groups, with signs and symptoms appearing at different ages, and varying in severity.








